My donor is incompatible, now what?
The best option for those with renal failure is a preemptive living donor kidney transplant. Unfortunately, many patients have family members or friends that wish to donate but preliminary testing reveals that they are either blood type or tissue type (HLA) incompatible.
In this situation, patients and their donors have two options:
There are two large nationwide donor exchange programs in the United States:
Desensitization
If a transplant is done in the setting of preformed antibodies, the graft will be lost to hyperacute rejection. Current strategies to remove antibodies have evolved over the last three decades and now achieve excellent results for ABO incompatible transplants. Unfortunately, these protocols have never been compared in clinical trials to determine the best approach. The general approach is to remove antibodies with plasmaphersis/ IVIG, and then keep them from being formed by using other drugs.
The antibodies titers are reduced prior to transplantation to allow a compatible crossmatch. Additional immunosuppression is used after the transplant to keep the titers low until accommodation occurs. This typically takes two weeks. The therapies include plasmapheresis, IVIG, and rituximab. The cost of these transplants is higher and there is a higher risk of rejection and infection. The additional cost depends on the protocol but it is still lower than the cost of chronic dialysis.
The new kidney allocation system allows for donation of kidneys from an A2 deceased donor to blood type B recipients as long the the A2 titer is checked and falls below a certain threshold. This should reduce the waiting time for blood type B recipients. The recipient who's living donor has an A2 blood type may not require desensitization if the titer is low.
Tissue type (HLA) incompatible transplants are more challenging. There are often many mismatched antigens. Multiple high level antibodies are difficult to eliminate and accommodation is less likely to occur. These patients are better served by donor exchange, especially if they are also ABO incompatible. Again desensitization is better than staying on chronic dialysis, especially if the waiting time for a deceased donor kidney is very long.
In this situation, patients and their donors have two options:
- enter a donor exchange program to find a compatible donor.
- undergo desensitization to remove the incompatible antibodies
There are two large nationwide donor exchange programs in the United States:
Transplant Candidates
that are receiving care at a U.S. transplant hospital, and are on
the national organ transplant waiting list can join. They do not have to be on dialysis but must have a living donor who is willing to donate a kidney. The donor must be at least 18 years old and be willing to take part in a paired donation.
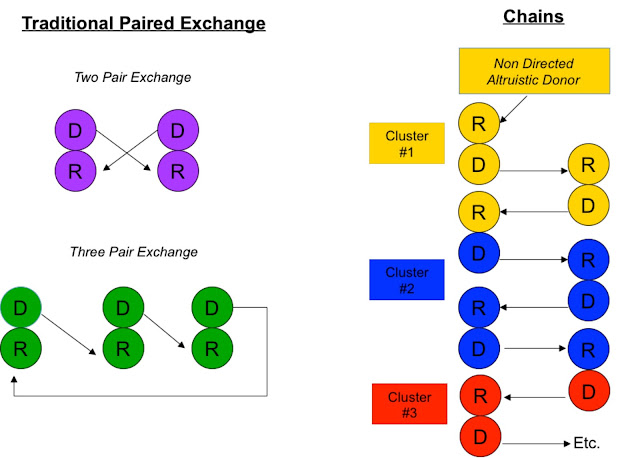
People who wish to donate a kidney to someone they don’t know are called non-directed,
altruistic or Good Samaritan donors. These donors are encouraged to enter these exchanges to help start and continue transplant chains.
Desensitization
If a transplant is done in the setting of preformed antibodies, the graft will be lost to hyperacute rejection. Current strategies to remove antibodies have evolved over the last three decades and now achieve excellent results for ABO incompatible transplants. Unfortunately, these protocols have never been compared in clinical trials to determine the best approach. The general approach is to remove antibodies with plasmaphersis/ IVIG, and then keep them from being formed by using other drugs.
The antibodies titers are reduced prior to transplantation to allow a compatible crossmatch. Additional immunosuppression is used after the transplant to keep the titers low until accommodation occurs. This typically takes two weeks. The therapies include plasmapheresis, IVIG, and rituximab. The cost of these transplants is higher and there is a higher risk of rejection and infection. The additional cost depends on the protocol but it is still lower than the cost of chronic dialysis.
The new kidney allocation system allows for donation of kidneys from an A2 deceased donor to blood type B recipients as long the the A2 titer is checked and falls below a certain threshold. This should reduce the waiting time for blood type B recipients. The recipient who's living donor has an A2 blood type may not require desensitization if the titer is low.
Tissue type (HLA) incompatible transplants are more challenging. There are often many mismatched antigens. Multiple high level antibodies are difficult to eliminate and accommodation is less likely to occur. These patients are better served by donor exchange, especially if they are also ABO incompatible. Again desensitization is better than staying on chronic dialysis, especially if the waiting time for a deceased donor kidney is very long.





Comments
Post a Comment